If you want things done right, sometimes you have to do it yourself. And sometimes “doing it yourself” means shifting the whole attitude of a worldwide effort.
Sage Bionetworks, a Seattle-based health nonprofit, supports collaborative and community-verified medical research. They manage consortia who share research and link academic and commercial researchers. They recently agreed to lead a national effort called the Open-AD [Alzheimer’s Disease] Drug Discovery Center.
The center is part of a two-pronged effort launched by the National Institutes of Health (NIH) to speed up and diversify research on Alzheimer’s. It will be led by Allan Levey, M.D., Ph.D., Emory University, Atlanta; Lara Mangravite, Ph.D., Sage Bionetworks, Seattle; and Aled Edwards, Ph.D., Structural Genomics Consortium. Their mission is to develop open-source tools and data for research and build a portfolio of drug targets based off prior NIH-funded research.
The “open source” part of the project is what’s (somewhat) revolutionary. Typically, researchers don’t share their methods or data; in the case of for-profit companies, that would be counterproductive, and historically, the majority of Alzheimer’s research has been performed by the biomedical industry. NPQ’s Amy Costello has interviewed epidemiologists working on massive disease outbreaks who lament the proprietary attitude of many researchers and medical workers, which ultimately hinders their effectiveness.
That’s what Sage Bionetworks and this new center will (hopefully) overcome. NIH director Dr. Francis Collins said, “Through these centers, NIH will expand the use of open-science and open-source principles to de-risk novel drug targets with the goal of facilitating the development of new treatments for Alzheimer’s.”
Sign up for our free newsletters
Subscribe to NPQ's newsletters to have our top stories delivered directly to your inbox.
By signing up, you agree to our privacy policy and terms of use, and to receive messages from NPQ and our partners.
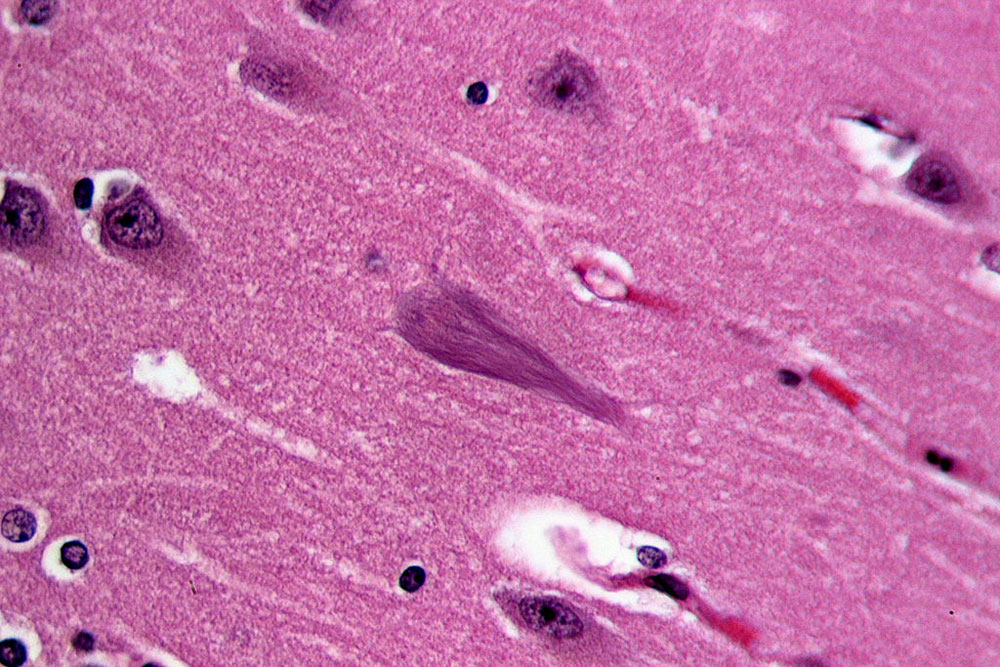
Alzheimer’s is considered by the NIH to be “among the greatest public health challenges of the 21st century.” It currently affects over five million people, and that number is expected to nearly triple by 2050. It’s a debilitating and expensive disease, and there is no known cure. Between 2002–2012, only .04 percent of trials resulted in a drug approval. And even available drugs don’t help everyone; the National Institute on Aging’s program director for Alzheimer’s Translational Research said, “We have been trying to treat AD as a monolith, but in reality it is not one disease. You can have 10 people…but processes driving their disease may all be different.”
So along with Sage, Emory University, and others, the NIH will pursue collaborative research, allowing scientists to share methods, data, and results to speed up the work on a cure.
The new centers will join other large research consortiums and efforts that recognize how collaboration aids science. The Bill and Melinda Gates Foundation has had an open access policy since 2015, requiring grantees to make their publications discoverable and accessible under a Creative Commons license. The Gordon and Betty Moore Foundation has one, too. And of course, the Electronic Frontier Foundation champions the use of open source software more broadly.
In a related field, research on amyotrophic lateral sclerosis, or ALS (Lou Gehrig’s disease) suffered a similar network failure: learning was happening, but in labs that didn’t communicate with each other. Kevin Gosnell, a Boston entrepreneur, founded ALS ONE to bring researchers together to share their learning. Gosnell pointed out that researchers weren’t just hiding potential avenues of success; they were hiding their failures, which meant money and time was spent on redundant research. Open source research can help alleviate that problem.
In May, NPQ’s Steve Dubb wondered whether nonprofits would eventually take over the field of antibiotic production, because the costs that pharmaceutical companies charge to make back their research expenditures creates an impossible binary of unaffordable medications and cash-starved labs. Is there a similar dynamic at play in major disease research? The five drugs that have been approved to treat Alzheimer’s in the past 26 years represent billions of dollars in research, and they only treat symptoms, not the disease. Is it even possible that a for-profit pharma company could produce and market an effective but affordable treatment without heavy nonprofit or government subsidy?
Sage Bionetworks’ Director of Neurodegenerative Research Ben Logsdon writes that exploring a successful research path for Alzheimer’s “requires a fundamental shift in how we think about doing science, because no individual contributor can perform all of the tasks necessary to expand our collective knowledge in a meaningful manner.” In some ways, he describes the work of our sector: a fundamental shift to a collective approach to make real change in the world. We wish them luck.—Erin Rubin