November 15, 2017; Grantmakers in Health
In the monthly e-newsletter of Grantmakers in Health (GIH), a trade association of funders dedicated to promoting “better health through better philanthropy,” Pritpal Tamber, cofounder and CEO of Bridging Health & Community, a Seattle-based nonprofit, calls on GIH members to not just fund programs, but people, if they wish to improve health outcomes at a systemic level.
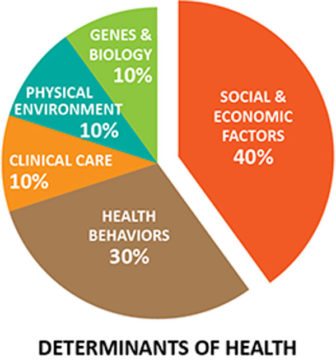
While Tamber and his colleagues are strong proponents of addressing the root causes or social determinants of health (such as poverty and environmental hazards), Tamber cautions that, “There is a risk that initiatives resulting from the health sector’s growing enthusiasm for influencing social determinants will be too limited to meet the mark because they leave out the knowledge and power of those most affected by the very challenges they intend to address.”
Bridging Health & Community was founded in 2013. Earlier this year, it hosted a symposium in Oakland, California, that brought together nearly 100 people to discuss the challenges and opportunities to foster community agency. Case studies looked at two efforts in particular, the Bronx Healthy Buildings Program, led by the Northwest Bronx Community and Clergy Coalition; and the Building Healthy Communities program site of South Kern County (south of Bakersfield), a 10-year community effort supported by The California Endowment.
Sign up for our free newsletters
Subscribe to NPQ's newsletters to have our top stories delivered directly to your inbox.
By signing up, you agree to our privacy policy and terms of use, and to receive messages from NPQ and our partners.
Tamber notes that the public health field faces some ironies. One the one hand, public health concepts such as “population health” (i.e., keeping people healthy) and “value-based health care” (i.e., changing compensation to focus on improving health, rather than the number of medical procedures performed) have gained in prominence. But the conversation remains driven by health sector professionals.
“As long as the health sector is the main driver of the conversation,” Tamber asserts, the resulting work will drift toward treating sickness, rather than promoting overall community wellbeing.
After four years of work informed by over 100 practitioner interviews, Bridging Health & Community has identified a set of 12 “guiding principles for what it means to genuinely and effectively work with communities. The principles,” adds Tamber, “describe a way of working—new to many in health—that is inclusive, participatory, and responsive.” These principles are:
- Include in a community’s collective effort those who live there, those who work there, and those who deliver or support services provided there.
- Spend time understanding differences in context, goals and power.
- Appreciate the arc of local history as part of the story of a place.
- Elicit, value, and respond to what matters to community residents.
- Facilitate and support the sharing of power, including building the capacity to use it and acknowledging existing imbalances.
- Operate at four levels at the same time: individual, community, institutional, and policy.
- Accept that this is long-term, iterative work.
- Embrace uncertainty, tension, and missteps as sources of success.
- Measure what matters, including the process and experience of the work.
- Build a vehicle buffered from the constraints of existing systems and able to respond to what happens, as it happens.
- Build a team capable of working in a collaborative, iterative way, including being able to navigate the tensions inherent in this work.
- Pursue sustainability creatively; it is as much about narrative, process, and relationships as it is about resources.
Tamber also calls attention to limits in how health is conceptualized. “Risk factors, Tamber observes, “whether personal, environmental, or social—explain less than half of why people are healthy or sick. The rest seems to come down to whether they have a sense of control over their lives, which requires agency. And yet we rarely see fostering agency embedded in work trying to influence health.”
Tamber closes with the admonition that, “Without an explicit focus on agency, most current work on social determinants of health is likely to fail. It will become yet another strategy subverted by seeing it only through the lens of the health sector.” To be successful, health philanthropy, Tamber says, does not just need to provide “patient, long-range capital,” but must shift how we conceive of the health enterprise itself.—Steve Dubb