June 26, 2018; RevCycleIntelligence.com
For health care providers and hospitals, just treating patients may not be good enough. Increasingly, experts have seen the need to view health in a larger, societal context. The American Hospital Association has recognized that people’s health is heavily influenced by the overall context of their lives.
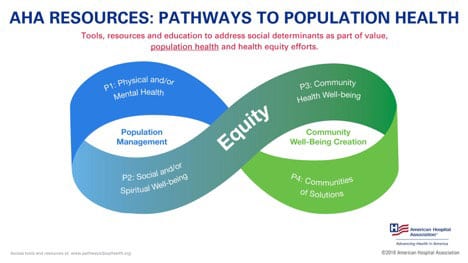
To meet medical objectives and to reduce the overall cost of health care, the American Hospital Association now advises its members that the “social determinants of health—where we live, work and play—have tremendous effect on one’s health, and they can affect anyone, regardless of age, race, ethnicity.” And it is urging hospitals to become engaged in efforts to change this larger picture.
According to a recent article on RevCycleIntelligence.com, a patient’s overall health is more dependent on the quality of their overall circumstances of their lives than it is on the quality of the health care they receive or on the accessibility of health care services. “Socioeconomic factors are responsible for approximately 40 percent of a patient’s health, while just 20 percent was tied to care access and quality of care.”
Being homeless, living in unsafe or unhealthy conditions, lacking transportation to get to needed medical appointments, or living in a food desert effects health more significantly than being able to see the best doctor or be treated in the finest hospital.
Sign up for our free newsletters
Subscribe to NPQ's newsletters to have our top stories delivered directly to your inbox.
By signing up, you agree to our privacy policy and terms of use, and to receive messages from NPQ and our partners.
With pressure from all quarters to reduce the cost of health care, hospitals and health care providers are motivated to build partnerships with other service providers toward improving the larger context of their patient’s lives. The AHA advises its members to invest in network building: “Knowing that hospitals and health systems alone cannot address all of these issues, external partnerships will be critical. Externally, hospitals and health systems can partner with other stakeholders or make other investments in their communities. This allows hospitals to not only serve as part of the solution, but to work with other stakeholders to better use limited resources to match the needs of their communities.”
Recognizing that many patients enter care with nutrition deficits, “organizations should also consider investments in food systems, such as food banks, local pantries, grocery stores, and farmers…establish community gardens, and allow food stands from local farmers on their property.”
Homeless individuals are heavy and regular emergency room users. Helping them leave the streets and enter stable, safe housing requires skills and resources outside the health care system. RevCycleIntelligence.com cited the University of Illinois Medical Center as a dramatic example of a service network addressing homelessness. The Center partnered with a community group called the Center for Housing and Health:
Hospital providers identified emergency department patients who were experiencing chronic homelessness and referred them to the community group. A panel of physicians, social workers, and other experts would then determine each applicant’s needs and pair qualifying individuals with an outreach worker who connects the individuals with the needed services. Individuals who accept the hospital’s help move into a “bridge unit,” or transitional housing unit, and case managers develop long-term solutions for independent living.
Hospitals’ openness to forming partnerships like these presents an opportunity for a range of organizations that focus on community improvement. Effective initiatives will require each partner to look beyond its own needs and see the work’s overall context. With each sector of the service community already under fiscal pressure as funding becomes harder to get and maintain, everyone needs to be concerned about more than the individual bottom line. The ongoing well-being of each partnership is important if the array of needed support services and community interventions will continue.—Martin Levine











