In an October 31 briefing, the Africa Union’s health watchdog issued a warning about the continent’s ongoing mpox outbreak, which started in early 2022. “The situation is not yet under control, we are still on the upward trend generally,” stated Ngashi Ngongo from the Africa Centres for Disease Control and Prevention (Africa CDC).
This follows the declaration in August by the World Health Organization (WHO) Director-General, Dr. Tedros Adhanom Ghebreyesus, that “the upsurge of mpox in the Democratic Republic of the Congo (DRC) and a growing number of countries in Africa constitute[d] a public health emergency of international concern (PHEIC) under the International Health Regulations (2005) (IHR).”
But in Sierra Leone, in West Africa, a coordinated effort across health agencies and nongovernmental organizations (NGOs) is preventing the virus from taking hold.
Understanding Mpox
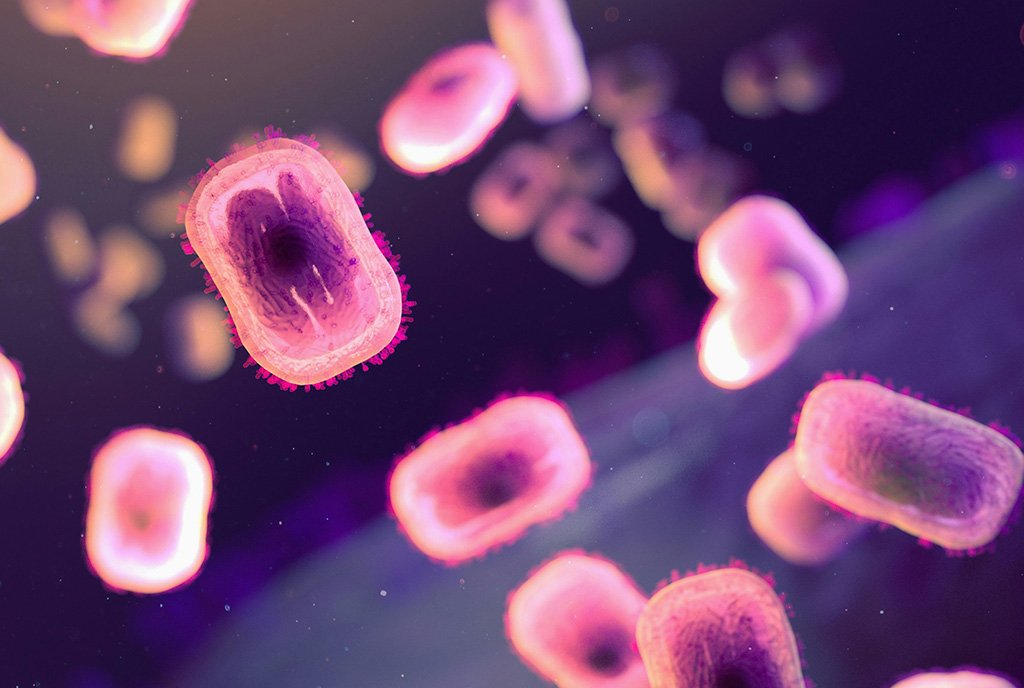
The outbreak in West Africa was part of a global resurgence of this disease, formerly known as monkeypox. Mpox is a viral illness causing fever, rash, and swollen lymph nodes, often spread through direct contact with bodily fluids or skin lesions.
While most people recover from mpox in a few weeks, individuals with weakened immune systems can suffer complications. Open lesions can invite secondary bacterial infections, increasing the risk of cellulitis, sepsis, or pneumonia.
In some severe cases, mpox may affect the respiratory system, causing bronchopneumonia. If untreated, the virus can lead to encephalitis or eye infections, risking vision loss. Prompt medical care reduces complications and aids recovery, especially for those at higher risk.
The recent outbreak in Africa has raised concern due to increased transmission in urban areas, affecting communities with limited access to healthcare. Sierra Leone is one of the countries with such vulnerability, with growing urban areas with limited access to healthcare.
The Current Mpox Situation in Africa
Nonprofits have been instrumental in improving healthcare in Sierra Leone.
As of October 2024, according to a situational report by WHO, 16 African countries continue to report new mpox cases. The DRC remains one of the most affected countries, with over 6,000 confirmed cases and 25 deaths. The resurgence in urban areas poses additional challenges due to higher population densities and increased mobility.
Neighboring countries have also been impacted. In September, neighboring Guinea reported the first case of mpox there, raising concerns about cross-border transmission. With many African nations sharing porous borders and limited resources for disease surveillance, coordinated regional efforts are crucial.
Containing Mpox
In Freetown, the capital of Sierra Leone, local and international health agencies have been working to contain the outbreak, with vaccination campaigns and public awareness efforts targeting high-risk groups. Many nonprofits in Sierra Leone that partner with the government to prevent a wider outbreak have so far been successful.
The National Public Health Agency (NPHA) and Ministry of Health (MOH), along with partnering organizations like UNICEF, activated emergency preparedness strategies while the outbreak was occurring in neighboring countries.
Dr. Vandana Joshi, chief of health and nutrition at UNICEF Sierra Leone, explained how the preparedness helped them contain the outbreak.
“We activated our Emergency Committee to respond,” Joshi explained, “We also quickly put together a response strategy and plan that addresses health, supply, social and behavioral change, and health information and awareness.”
UNICEF’s response strategy aligns with the NPHA’s three-month mpox contingency plan, which focuses on preventing mpox cases in neighboring countries from spreading into Sierra Leone.
“UNICEF put in place sustainable means of reducing disease through regular hand washing with soap in schools, health centers, and communities, pre-positioning supplies that can be rapidly deployed,” Joshi added.
Sign up for our free newsletters
Subscribe to NPQ's newsletters to have our top stories delivered directly to your inbox.
By signing up, you agree to our privacy policy and terms of use, and to receive messages from NPQ and our partners.
Part of the UNICEF strategy helped bolster the ongoing efforts by the NPHA to prevent mpox from spreading. Although there were no reported cases in Sierra Leone as of August 2024, the government preemptively increased checks at entry points in airports, seaports, and areas along its border; disseminated additional educational pamphlets that informed vulnerable areas; and helped regular meetings with nonprofit, nongovernmental agencies to align its preparation strategies.
“Many good lessons were learned from the 2014–15 Ebola pandemic in terms of preparedness and response, and these are being incorporated into this mpox preparedness and response strategy.”
The Role of Nonprofit Organizations
Freetown serves as a hub for many nonprofits and NGOs dedicated to improving healthcare and supporting development initiatives. Because of the country’s pressing need for development assistance and its history of challenges that require international support, international organizations often establish their administrative headquarters in the city.
Nonprofits have been instrumental in improving healthcare in Sierra Leone. During the 2014 Ebola outbreak, organizations like Médecins Sans Frontières (MSF) and the International Federation of Red Cross and Red Crescent Societies (IFRC) provided emergency care, training, and infection control support to curb the spread of the virus.
Their involvement significantly reduced infection rates and fatalities. Organizations like Partners In Health (PIH) focus on enhancing maternal and child healthcare, providing life-saving resources, and strengthening healthcare infrastructure. According to PIH, their work in Sierra Leone has reduced maternal mortality by 8 percent from 2020 to 2022.
UNICEF, an agency with a more permanent footprint in Sierra Leone, has successfully addressed critical health, education, and child protection challenges. The organization’s work in improving maternal and child healthcare has reduced child mortality through immunization programs, distributing insecticide-treated bed nets for malaria prevention, and improving access to clean water and sanitation. As a result, UNICEF has helped decrease mortality rates for children under five by more than 51 percent since 2000.
Addressing Misconceptions and Stigma
When preventing the spread of mpox, the virus isn’t the only focus. In UNICEF’s final internal report on mpox in Sierra Leone, shared with NPQ, the organization found “notable gaps in understanding of the transmission routes, symptoms, and preventive strategies related to Mpox.”
The report concluded, “Critical barriers include misconceptions, stigma, and a lack of awareness regarding the Mpox vaccine,” with “fear and stigma hinder[ing] open dialogue about the disease, especially in rural communities and among sex workers and young people.”
In a story on mpox by UNICEF Sierra Leone, the organization reiterated the need for public information campaigns to “reduce stigma associated with the virus.”
Sierra Leone’s success highlights the strength of a coordinated network of NGOs, government agencies, volunteer organizations, and an informed public.
According to The Guardian, millions of doses of mpox vaccines have arrived in the DRC, but many people are reluctant to get them: “Conspiracy theories spreading across the country include the suggestion that mpox has been invented by white people in order to sterilise Congolese people with vaccines—or that it is just a money-making scheme from pharmaceutical companies. Mistrust in medical institutions and treatments is in many cases a legacy of racist colonial policies.”
To combat this, the Ministry of Health has created multiple plans for educational programs and public awareness campaigns to correct misconceptions, promote vaccinations, and engage with community leaders.
“We collect surveillance data from hospitals and clinics with special focus on high-risk districts, and we supply information on identification and prevention of mpox with community health workers (CHWs) supported by UNICEF,” Joshi explained.
Looking Ahead
In many ways, Sierra Leone’s response to the mpox outbreak is a testament to the power of aligning nonprofit partnerships with a proactive public health strategy. Through swift action, community engagement, and effective healthcare interventions, the nation has controlled a potential crisis that could have escalated rapidly.
Sierra Leone’s success highlights the strength of a coordinated network of NGOs, government agencies, volunteer organizations, and an informed public—and underscores the importance of investing in public health infrastructure to protect communities locally and globally.










