December 4, 2020; CNBC
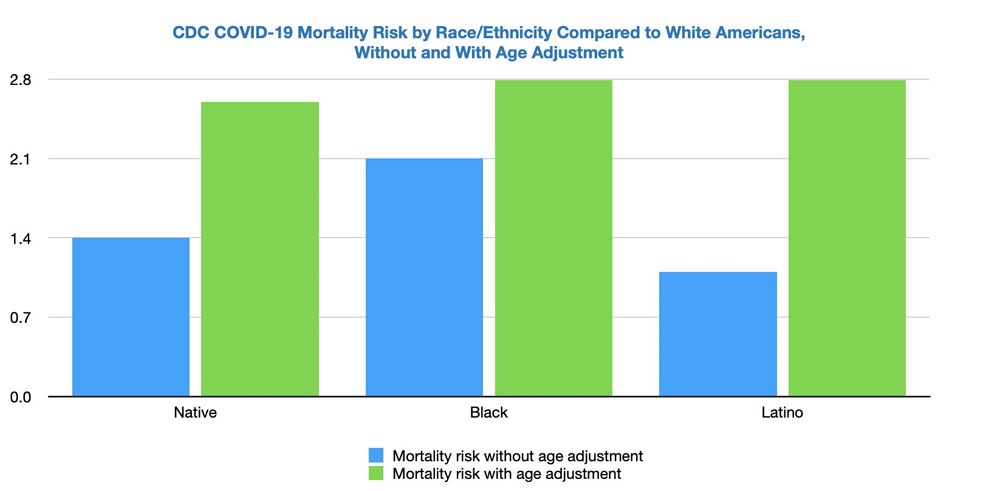
The US Centers for Disease Control and Prevention (CDC) concedes that its estimates were low when it said that Black and Latinx people were dying at rates 2.1 times higher than that of white Americans. After being challenged on their research methodology, which did not take age into account, they revised their estimate up to 2.8 times that of whites, far closer to estimates US Senator Elizabeth Warren (D-MA) had advanced. The new figure for Native Americans and Alaskan Natives is now set at 2.6 times that of whites, up from 1.4 times.
Update: @CDCgov got our request, and has adjusted its official COVID-19 race/ethnicity mortality rates for age. The data show that Black, Latino, and Native Americans are dying of COVID-19 at a much higher rate than white Americans than they previously indicated. https://t.co/LA8tvtOGu2 pic.twitter.com/cvTNWdPoJL
— Elizabeth Warren (@SenWarren) December 2, 2020
This revision followed challenges from a number of people, including Warren, who said the factor of age had not been properly handled. Adjusting for age has so strong an impact on the analysis because “people of color are, on average, significantly younger than non-Hispanic white Americans,” as Warren put it in her letter to Redfield, and older people are more likely to die of the coronavirus. An illustration of this: while the most common age for white Americans is 58, it’s 27 for Black Americans—and for Latinx persons, 11. The gap in median ages is, of course, far less, but still significant. The median white person is 44 years of age; the median person of color is 31 years of age.
Sign up for our free newsletters
Subscribe to NPQ's newsletters to have our top stories delivered directly to your inbox.
By signing up, you agree to our privacy policy and terms of use, and to receive messages from NPQ and our partners.
Dr. Leana Wen, former Baltimore health commissioner, and an emergency room physician and public health professor at George Washington University, says that without the age adjustment, estimating disparities is “comparing apples to oranges” and that race is less a deciding factor than is racism.
“I hope that people will see that it’s not the virus that’s doing the discriminating,” Wen said in a phone interview with CNBC. “It’s our systems.”
She explained that people of color are more likely to have jobs that deem them essential workers, for example, which increases their risk of exposure to the virus. She also said people of color are more likely to live in multi-generational housing, which could let the virus spread more easily from younger to older people.
Hospitalization data show a similar pattern as the data from the CDC documents. Between March 1st and November 28th, age-normalized hospitalization rates per 100,000 individuals are as follows:
| Latinx | 533.7 |
| American Indian/Alaskan Native | 521 |
| Black | 475.5 |
| Asian and Pacific Islander | 158.8 |
| White | 140 |
As the CDC reports, “When examining overall age-adjusted rates by race and ethnicity,” the rates for Latinx, Native American and Black Americans are respectively about 3.8, 3.7, and 3.4 times the rate of whites.
Why is the data so important? “It’s important for us to understand why it is that COVID-19 has unveiled and unmasked these underlying disparities,” Wen said. “There are short-term things that could be done. For example, targeting testing to areas that are the hardest hit, ensuring that resources, including vaccines, are targeted to these same communities, as well, while longer term, committing to working on the social determinants of health.”—Ruth McCambridge













