Editors’ note: This article is from NPQ‘s winter 2022 issue, “New Narratives for Health.”
The birth experience of expectant parents living in the tribal lands of rural Northern California can be harrowing. Everything from access to prenatal care to timing the journey to the hospital requires careful planning and savvy navigation of narrow roads and complex health systems. And that negotiation does not end at the hospital door. Rather, it shifts into a different sort of navigation: the too-common experience of being a Native person in a healthcare system that is mostly unaware of the historical trauma and cultural traditions that infuse the birth experience of Native people. Too often, the joy of a Native family’s birth experience is tainted by fear, ignorance, and racial bias.
Over the last year, parents and leaders from tribal lands in and around Humboldt County in Northern California and medical practitioners from the local Providence St. Joseph Hospital have been working to better the birthing experience of Native parents.1 This work emerged from the hospital’s efforts to improve health outcomes for Native people in partnership with that community—an effort that continues beyond the story told here.
Providence St. Joseph Hospital is a busy place. Like most hospitals across the country, it has been working intensely and relentlessly over the last three years of the pandemic to deliver care to those who live in and around Humboldt County. The hospital has a deep connection and commitment to the health of the community that extends beyond the doors of the hospital, and to the well-being of individuals. The hospital already had strong working partnerships with other communities, notably Latinx communities and also homeless populations, whose health disparities were strongly linked to their culture and existing societal inequities. This was not the case with tribal leaders and organizations, and the hospital’s CEO understood that the hospital needed to establish trusting relationships with these groups before the work on improving health outcomes could begin.
From its base on the coast, the hospital serves Native people who live and work on land of nine federally recognized tribes and Rancherias, among other communities. Native people make up over 6 percent of Humboldt’s total population, compared to just 1.3 percent nationally and 1.7 percent in California as a whole.2 The preservation and vitality of Indigenous culture of the Karuk, Hupa, Tolowa, Wiyot, and Yurok people have benefited from the geographic isolation on this “lost coast” in Northern California. And while they did not suffer complete displacement, the Native communities here still experienced genocide, family separation, and repercussions for openly practicing their traditions.3 It is only since 1978 that Native community members could openly practice their ceremonies and traditions in the United States.4
Before the “Better Birthing” team work began, Providence, which oversees St. Joseph Hospital, had made a significant financial and programmatic commitment to health equity.5 Providence staff responsible for the health equity portfolio were exploring human-centered design as a way to integrate community needs and boost creative solutions to local health equity challenges. There was growing understanding at Providence that the path to improving community health outcomes was highly dependent on the involvement of those most impacted—in this case, Native patients. Providence St. Joseph Hospital in Humboldt County was selected to receive funding for this work in part because staff had already recognized the need to increase relational trust with Native people on the path to improving health outcomes.
How it Happened: The Process of Community Codesign
The work of changing systems begins with creating greater visibility of how a system functions, who it benefits, and who it harms.
The core of the community codesign process that anchored the Better Birthing work will be familiar to those who know human-centered design.6 It began with lived experience interviews, sensemaking of those interviews with an eye to identifying opportunities for change, and then moved into ideation and prototyping to create and advance solutions. Unlike more traditional design approaches, the Better Birthing design process viewed the community as the designers of new solutions rather than solely informing the work. This meant that the work involved multiple people and organizations at every stage and that the project team comprised key stakeholders in the perinatal care system. The work is messy, nonlinear, and ongoing. For simplicity’s sake, we offer a high-level description of our learnings:
Map the system you are trying to change. All of us are constantly navigating multiple social systems: the education system, the healthcare system, our family system. It is challenging for anyone to see the full workings of any complex system. That is especially true if you are comfortable with your place in that system. The work of changing systems begins with creating greater visibility of how a system functions, who it benefits, and who it harms.
At the start of the Better Birthing work, Providence brought in an outside consulting team from the With/In Collaborative (the authors of this article) to map the systems that support a Native parent’s birthing experience.7 We spoke with dozens of stakeholders; discovered what organizations and people affect pregnant patients directly and indirectly; and, ultimately, created a visual of how these stakeholders are organized and connected to one another and to the hospital. We came to understand that the hospital was both geographically and physically distant from the birthing experience of many Native patients. Often, the hospital was the literal “last stop” for parents—who sometimes arrived at the hospital for the first time when already in labor—rather than a persistent player in the continuum of care during pregnancy.
Build a team that mirrors the people from within that system. The process of mapping the birthing system also helped to identify the people who should be intimately involved in the design work. The original Better Birthing team, nine members strong, included an obstetrician, a Native labor and delivery nurse, a Native childbirth educator, a community-based social worker, the head of the hospital’s NICU, Native parents, and Native elders. The team’s composition mirrored the tensions, power dynamics, and history that currently exist in the local birthing system. Native wisdom was put on an equal footing with medical expertise; and team members were recruited, in part, for their dissatisfaction with the current set of supports for Native parents and their ability to spur change across the community. By design, the team’s dynamics were a microcosm of what would need to be navigated more broadly in the system itself.
The act of interviewing Native parents as a team was a deeply moving shared experience that created a collective body of knowledge that was independent of any one person’s experience or expertise.
From the start, there was warranted skepticism by Native team members about the motivations and commitment of Providence St. Joseph Hospital and the consultants. One Native team member described it like this: “I felt unsure about this project and if this was just another way an [organization] was going to come in and say, ‘Oh, look at the great work we did,’ and then call it a day. I was also nervous about having outside consultants come in to work with a team. This all made me question joining this group. Would I be a pawn of exploitation?”
It was no small task for the team to hold their fears and suspicions while moving forward together, but the design process helped to relieve some of the tensions. To begin with, the team members spent time sharing their personal stories and identities, including how their own experience of birth informed the work that they do. We invited the team to come to meetings as themselves rather than as their expertise or job titles. This worked to reduce some of the power differentials within the group, and created a path for building relationships. Later in the process, the act of interviewing Native parents as a team was a deeply moving shared experience that created a collective body of knowledge that was independent of any one person’s experience or expertise. It is also clear that the hospital’s willingness to acknowledge its contribution to how systems at the hospital and in the community have created harm and perpetuated racial bias created goodwill in the team and the Native community.
That said, the tensions that existed at the beginning continued to show up in the team’s work with one another throughout the design process. This reality fueled our learning, often changed our approach, and served as a constant reminder that pain, guilt, sadness, and bias remain ever-present in the effort to change broken and historically racist systems. Especially for the non-Native team members, it was important to continually acknowledge that non-Native people will never fully understand the experience of Native people, even when moving forward together.
Deeply understand the stories of those most impacted by the system. The guiding force of the team’s work were the interviews that they conducted with eleven Native parents who had recently given birth.
Starting with deep listening to personal stories anchored our understanding about the birth and perinatal care experience of Native parents and fueled our thinking about what needed to change.
What the team heard from Native families was that they often experienced disconnection and fear alongside the joyous overwhelm of birth. We heard stories of Native parents struggling to support Native birthing traditions in a hospital environment. And we heard too many stories that featured cultural ignorance and missed opportunities for comfort and care. We came to understand through these stories that the experience of many Native parents giving birth at a hospital is intimately connected to the devastating history of how the state and institutions have treated Indigenous people in the last two centuries. As our team retold these stories to one another, we also came to believe that the institutional birth experience holds the possibility of repair and connection.
Native parents lean heavily on family and tribal support systems during their pregnancies and during the birth. They need advocates, doulas, and nurses who understand their community and traditions.
As one team member reflected: “It was really hard to hear what things occurred to patients. I wanted to learn all that I could to fix the situation, and it took time for me to understand that some things [(traditions, ceremonies, and so on)] are not appropriate for me to know as a non-Native person. I also can’t believe how I grew up and always lived in Humboldt County and never knew about the history and traditions of our Native communities.”
Move from stories to the parts of the systems you want to change. The team spent many hours unpacking the experience of each birth parent and the systems and services that affect them. The hope was to understand the barriers to and opportunities for improving each parent’s birth experience. Ultimately, the team’s sensemaking created clarity about what threads of work to pursue. Honoring what the team now understood was important to Native parents, we articulated three strategic areas that the team felt might be most impactful for parents:
- Increase the personal agency of birthing parents. Often, parents struggle to be heard during their birth experience. Patients need their wants and wisdom to be heard by hospital staff. Ironically, the team realized that the hospital also struggled to communicate to new parents what decisions they could make. There was a communication gap that created misunderstandings and fear.
- Support the presence and voice of Native advocates at the bedside. Native parents lean heavily on family and tribal support systems during their pregnancies and during the birth. They need advocates, doulas, and nurses who understand their community and traditions. During the pandemic, when the hospital had to severely restrict who could attend a birth, Native patients suffered. The team saw an opportunity for the hospital to create a more inclusive and supportive environment for Native patients by supporting and expanding the role of Native advocates, especially at the bedside.
- Cultivate cultural responsiveness institutionally at the hospital. Native parents struggle to integrate Native birthing practices with hospital protocols. Many birthing mothers experience discrimination, lack of cultural empathy, and pushback on practicing traditions from medical staff who are ignorant of their history. Birthing has the opportunity to be a moment of connection to culture and community support systems for Native parents. It is also an opportunity for the hospital to support that connection, instead of creating disconnection.
Shape the Interventions. Regarding the above three strategic areas, the team discussed and weighed multiple interventions to pursue. Some solutions were more clear and some less so. Some of the experiments moved forward but many didn’t. Admittedly, there was a lot of ambition without full clarity at the time about how things would unfold. The team brainstormed how they might address each strategic area and also who else should be involved from the hospital and from the community, because the viability of each experiment was highly dependent on having partners in the community with time, capacity, and interest to join in the work.
One experiment the team was eager to try focused on redesigning the intake interview that all birthing parents experience when they first arrive at the hospital, before they are admitted and placed in a birthing suite. The hope was to promote the birthing parent’s agency and the intake nurse’s cultural responsiveness by rethinking what questions might improve communication from the start. This idea quickly shifted after hearing from labor and delivery staff about the many constraints of that intake interview from the hospital’s point of view, including the realization that the interview was often conducted when the birthing parent was enduring the pain of labor. The experiment was redirected to focus on how we might educate both parents and medical staff about each other before patients arrive at the hospital. This early idea ultimately evolved into our redesigned birth plan (see below).
Sign up for our free newsletters
Subscribe to NPQ's newsletters to have our top stories delivered directly to your inbox.
By signing up, you agree to our privacy policy and terms of use, and to receive messages from NPQ and our partners.
What Happened Next: Multiple Efforts at Experimentation and Implementation
At this point, our original team of nine people became multiple teams that included community leaders and other organizations. There were about a half-dozen efforts under way simultaneously as we did our work— some very structured and time bound, others more exploratory and longer term. What ultimately emerged was a commitment to projects that seek to provide the care Native parents want versus what they have experienced in the past.
Some of the projects that moved forward were focused on filling knowledge gaps about Native people in the healthcare system. We created a one-page internal document for medical staff that describes how the history and traditions of Native people may influence their approach to their medical care. We organized trainings with a local Native midwife for labor and delivery staff to learn about Native birthing traditions. And we worked to disseminate what we learned from Native patients to other important stakeholders in the birthing system (lactation consultants, childbirth educators, family centers, and so forth). Ultimately, the team focused most of its time and capacity on three major areas of work. These included:
Changing California state law. Until recently, California state policy required that all families register the birth of a child with the hospital by the tenth day of life. This practice often conflicted with the period of sacred ceremonial blessing and naming of a newborn in local Native communities on the tenth day.
The effort to change state policy emerged from the stories told to the Better Birthing team by Native parents and by hospital administrators. We heard from parents how offended they were by the constant requests by hospital staff to reveal their newborn’s name before they left the hospital. In turn, hospital staff were frustrated that their attempts to prevent families from incurring the additional cost and paperwork involved if parents missed the ten-day deadline to register their child were experienced as ignorance and cultural insensitivity.
Changing state policy was not something that the Better Birthing team could do alone. Team members from the hospital recruited the government affairs team at Providence to determine the viability of this effort. The head of Providence’s team then arranged for members of the Better Birthing team to present their findings to California State Assembly member Jim Wood, who agreed to draft the legislation and steward the effort through the state legislature. Ultimately, the team solicited over forty letters of support from local and statewide tribes, healthcare organizations, and leaders before it went before the state assembly; and Native parents allowed the Native doctor and the tribal council member—who ultimately provided testimony to lawmakers—to tell their birth stories. As one team member reflected: “I liked that the hospital was able to use their power to lift up local Native voices and experiences, even though this action did not directly benefit the hospital.”
With an eye to promoting better communication and cooperation between parents and the hospital, the Better Birthing team experimented with using a birth plan.
On June 22, 2022, California Governor Gavin Newsom signed CA Assembly Bill 2176 into law.8 This bill extends the time all families have to register the birth of their child, from ten days to twenty-one days.9 This new law removes that irritant in the relationship between Native patients and medical staff; more important, it signals the willingness of the state to be more respectful of sovereign First Nations practices.
Leveraging a parent’s birth plan to cocreate a culturally responsive birth environment. Many Native parents we interviewed described feeling unwelcome upon arriving at Providence St. Joseph Hospital, nervous about how they would be received and unclear about what choices they had regarding the birthing experience there. We heard from parents that they felt that traditional baby baskets, food, and medicinal plants were not welcome at the hospital. Others had concluded that the hospital was racist after being administered a drug test at intake—when in fact that test is administered to all birthing parents.
With an eye to promoting better communication and cooperation between parents and the hospital, the Better Birthing team experimented with using a birth plan. Birth plans, which typically express a parent’s hope for the birth experience and make requests of the medical team, are not a new idea. But those hopes and requests are often out of sync with the hospital’s requirements or the medical realities of that parent’s birth experience.
The redesigned birth plan attempts to bridge the gap in cultural responsiveness and knowledge between parents and the medical team. We found that, typically, the medical staff present at a birth are unaware of how a patient’s race, ethnicity, or religion impacts their decision making and preferences. The redesigned birth plan prompts parents to describe how their traditions influence their decision making around the birth experience. For example, if it is the Native parents’ tradition to keep the placenta or umbilical cord, the birth plan prepares parents to bring a cooler for storage; sign a specific form of release; and designate a family member for transport. The birth plan is also an opportunity for the hospital to express its support of Native traditions by declaring, for example, that Native baby baskets and traditional medicinal plants are welcome in the birthing rooms.
Likewise, parents are often unaware of which hospital procedures are elective versus required. The birth plan makes explicit what is standard medical practice at Providence St. Joseph Hospital. It provides clear decision points, so that parents can decide on their preferences ahead of time—for example, to have either intermittent or constant baby monitoring, or whether or not to have an intravenous lock for medical interventions when it’s not clearly warranted.
How to use and integrate the new birth plan is still a work in progress at prenatal clinics and at the hospital itself. And the team is interested in adapting the birth plan to also reflect the needs and language barriers of the Spanish-speaking populations in the community. Ultimately, the goal is for the birth plan to become a way for local care providers to express their cultural responsiveness and questions in a way that invites more collaboration with the birthing parent.
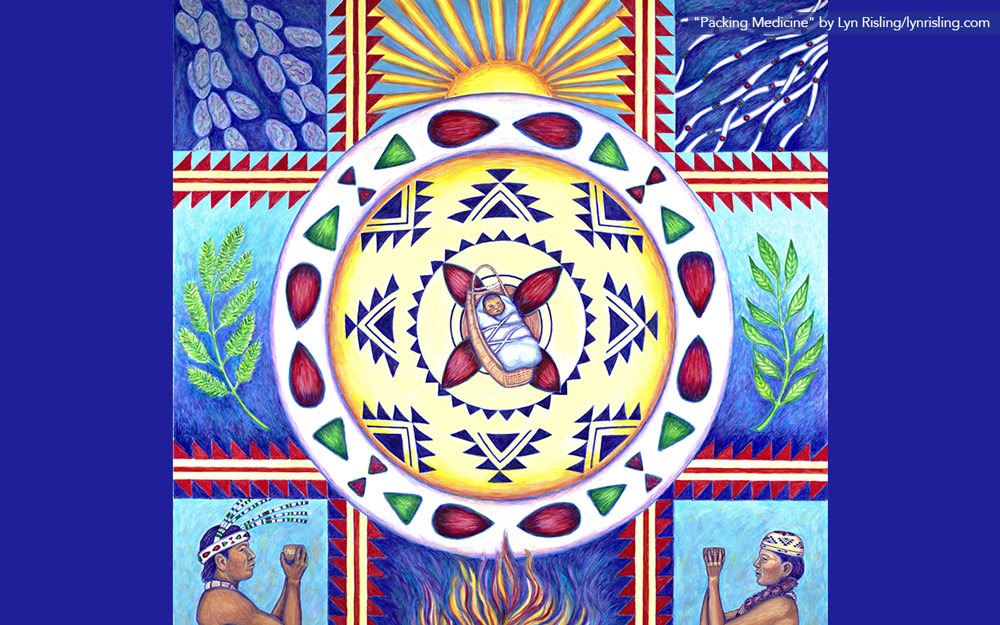
Changing the hospital environment to reflect the communities it serves. As luck would have it, the hospital had recently received funding to remodel its birthing unit just as the Better Birthing team began its work. This allowed the hospital administration to address early feedback the team had received from parents and members about what it felt like to be at the hospital as a Native person. Parents observed that the pictures hanging on the walls did not reflect the cultures of all those giving birth there, and that the birthing unit felt sterile and institutional.
The Better Birthing team, other Native leaders, and representatives of the local Latinx, Black, and Hmong community worked with the hospital to create a space that was more representative of the community. They suggested that the hospital bring elements of the incredible rivers and trees of Humboldt County into the space for both inspiration and because it “felt like home.” The team selected pictures for the walls that were not only racially representative but show women breastfeeding and men nurturing their newborns. Finally, the hospital was able to purchase incredible artwork from Native local artists that reflects Native traditions.
The Work Continues
Beyond these concrete attempts to shift the birthing experience of Native parents, the hospital is continuing to build relationships with tribal leaders and Native patients on the path to addressing health disparities in the community together. Internally, the hospital is experimenting with how it can provide high-quality care that embeds more cultural responsiveness through staff training (especially staff new to the community) that prioritizes respect for patients and understanding of local populations. And externally, the hospital is looking to connect with parents before they arrive at the hospital to give birth. The hospital now sends two labor and delivery nurses at a time to clinics in Native communities to participate in prenatal care and education. This partnership was the idea of a local Native parent, who then brokered the partnership between the hospital and the clinic.
The work of the Better Birthing team is also continuing to evolve. Recently, the team received the 2022 Leighton Memorial Award by the CARESTAR Foundation for its success in addressing inequity in hospital care in a rural or tribal community.10 Beyond the immense honor of receiving the award, it also funds the expansion of the Better Birthing work. The team has decided to focus the next chapter of its work on culturally informed postnatal care for Native parents.
***
The ultimate aspiration of this work is to redesign a more equitable healthcare system that will improve health outcomes for all. While we are far from claiming victory, we did land on a core belief that the work of changing systems occurs at the intersection of relational, actionable, and systemic work with those deeply embedded in the system itself. To the Better Birthing team, this meant giving time and space to truly understanding the current and historical impact of our communal systems on those most affected; committing to building relationships through concrete work together; and aligning solutions with people’s needs.
In the case of Humboldt County, the work of building relational capital and trust through deep listening and joint project work has begun to shift how Providence St. Joseph Hospital and the surrounding Native communities relate to one another. It has not gone unnoticed that the hospital used its power to lift up Native voices in the community and across California. Native team members have reflected that this work has given them hope for a different future; but they also caution that this is just a small step of repair in a system that has perpetuated harm toward Native people for hundreds of years, and will mean little if it does not continue apace. To those in pursuit of just systems that equitably serve all, this is a reminder of both the hope and the realities ahead.
In addition to the many tribes, Rancherias, organizations, and individuals who provided letters of support for AB2176, we would also like to thank K’ima:w Medical Center, United Indian Health Services, Two Feathers Native American Family Services, the Yurok Tribe, and the Native parents who provided guidance on the Better Birthing journey.
Notes
- Alana Minkler, “Bill passes extending birth registration, accommodating Native American traditions,” Press Democrat, June 29, 2022, www.pressdemocrat.com/article/news/bill-passes-extending-birth-registration-accommodating-native-american-tra/.
- QuickFacts: California; United States, “Population Estimates, July 1, 2021”; and QuickFacts: Humboldt County, California, “Population Estimates, July 1, 2021” data derived from the American Community Survey Population Estimates and other databases, Bureau of the Census (Washington, DC, 2021), www.census.gov/quickfacts/fact/table/CA,US/PST045221 and www.census.gov/quickfacts/humboldtcounty california, respectively.
- “History of Native California,” Native American Studies, College of Arts, Humanities and Social Sciences, Cal Poly Humboldt University, video, 12:58, accessed December 30, 2022, humboldt.edu/files/history-native-california; and Gavin Rowley, “Defining Genocide in Northwestern California,” Humboldt Journal of Social Relations 42 (August 2020): 87–105.
- American Indian Religious Freedom Act, 42 S.C. § 1996 (passed 1978), coast.noaa.gov/data/Documents/OceanLawSearch/Summary%20of%20Law%20-%20American%20Indian%20Religious%20Freedom%20Act.pdf.
- “Providence commits $50 million to address racial disparities in health care,” News, Providence, September 1, 2020, providence.org/news/uf/628030088.
- Thomas Both, “Human-Centered, Systems-Minded Design,” Stanford Social Innovation Review, March 9, 2018, ssir.org/articles/entry/human_centered_systems_minded_design#.
- See With/In Collaborative, withincollaborative.com.
- Jackson Guilfoil, “Gavin Newsom signs Jim Wood bill extending birth registration deadline,” Times- Standard, June 23, 2022, times-standard.com/2022/06/23/gavin-newsom-signs-jim-wood-bill-extending-birth-registration-deadline/.
- Minkler, “Bill passes extending birth registration.”
- “The CARESTAR Foundation Awards $100,000 Leighton Memorial Award to the Better Birthing Coalition,” Cision PR Newswire (blog), September 13, 2022, prnewswire.com/news-releases/the-carestar-foundation-awards-100-000-leighton-memorial-award-to-the-better-birthing-coalition-301622560.html.










