November 20, 2017; American Prospect
Life expectancy in 14 of Baltimore’s predominantly Black neighborhoods is now lower than North Korea’s, notes Jim Grossfeld in the American Prospect. This is true even though, as Grossfeld points out, Baltimore is home to Johns Hopkins, which, Grossfeld observes, “Together with the Mayo Clinic and the Cleveland Clinic…is part of the trinity of top-ranked US hospitals—a latter-day Lourdes to which sick people from around the world beat a path, hoping to find cures they’ll find nowhere else.”
Why does proximity to a top-flight hospital matter so little? “There is a difference between health care, which is critically important, and the array of social, economic, and environmental determinants of health,” says Dr. Brian Smedley, co-founder and executive director of the National Collaborative for Health Equity. “In fact, the health of populations is only minimally affected by health care.”
The Baltimore City Health Department, in its “Healthy Baltimore 2020: A Blueprint for Health” report, points out that “although 97 percent of health-care dollars are spent on the health-care system, only 10 percent of what determines life expectancy actually happens ‘within the four walls of a clinic.’ The other 90 percent is decided upstream, where people live, work, go to school, and spend their free time.”
And those “upstream” factors, which often are referred to as social determinants of health, are heavily influenced by poverty and racism. Regarding poverty, Grossfeld notes that in Baltimore, a city with a Black majority, “more than 28 percent of African Americans in the city live below the poverty line. The poverty rate for Baltimore households headed by women—the vast majority of whom are African American—is far higher, 41 percent.”
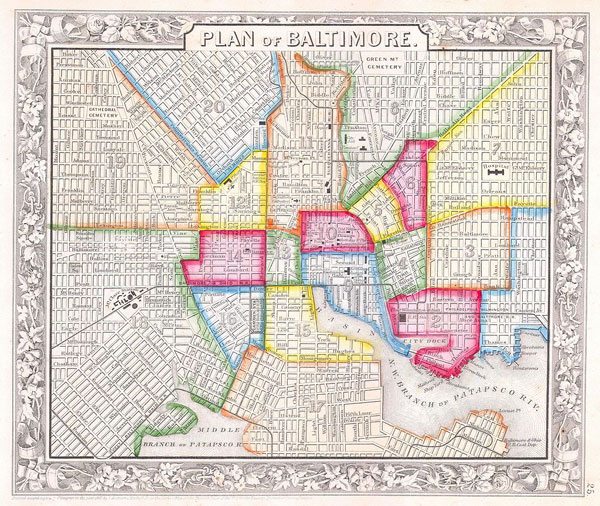
Structural racism runs deep in Baltimore. A 1911 Baltimore City ordinance read, “Blacks should be quarantined in isolated slums in order to reduce the incidence of civil disturbance, to prevent the spread of communicable disease into the nearby White neighborhoods, and to protect property values among the White majority.”
In 1937, the official federal government Baltimore “residential security” map—better known as the redlining map—marked Black neighborhoods with red “do-not-lend” shading. And these dividing lines remain with us still; as a 2015 City Lab article on Baltimore points out, there is “a striking alignment of today’s poverty rates and the Nuremberg-like government mortgaging practices of the 1930s.” As Gallagher remarks, “these numbers provide as much insight into the health crisis facing African American neighborhoods as MRIs or CT scans of the individuals living within them.”
Sign up for our free newsletters
Subscribe to NPQ's newsletters to have our top stories delivered directly to your inbox.
By signing up, you agree to our privacy policy and terms of use, and to receive messages from NPQ and our partners.
Indeed, nearby neighborhoods can have very different health outcomes: Madison/Eastend is 90 percent Black and has an average life expectancy of less than 69 years, while nearby Medfield/Hampden/Woodberry/Remington, which is 78 percent white, has a life expectancy of 76.5 years. If you break this down, Madison/Eastend’s homicide rate is nearly 12 times higher than Medfield, its cancer mortality rate is 66 percent higher, and its AIDS mortality rate is more than 12 times higher.
Grossfeld also emphasizes the health impact of police violence, which sharply elevates stress levels in Black communities. Grossfeld notes that two thirds of young Blacks “say that they or someone they know has experienced violence or harassment at the hands of the police.” It is estimated that nearly one in ten Blacks “suffer from post-traumatic stress disorder.”
An additional challenge is the paucity of Black doctors, which nationally runs at five percent, with few signs of change in the offing. And the gap is important: Gallagher notes that Dr. David Ansell and Dr. Edwin McDonald reported in a 2015 New England Journal of Medicine article that, “Black medical students are more than twice as likely as white students to express a desire to care for underserved communities of color. Our inability to recruit Black men into medicine is alarming, given the urgency of racial health care disparities in the United States.”
On a brighter note, Gallagher does cite some evidence of positive responses to these challenges. For example, Gallagher observes,
One group working to counteract these trends is White Coats 4 Black Lives, or WC4BL, a national organization of medical students whose mission is “to eliminate racial bias in the practice of medicine and recognize racism as a threat to the health and well-being of people of color.” With 54 active chapters at medical schools across the nation, WC4BL says its primary goal, in the spirit of Black Lives Matter, is to put medicine’s racial disparities on the front burner.
Santiago Ali, a former EPA senior advisor and now a senior vice president at the Hip Hop Caucus, observes that the water crisis in Flint, Michigan, has helped bring together environmental justice and public health advocates, along with Black Lives Matter activists. Noting that community health centers today serve 24 million in low-income communities, Ali suggests that this is a foundation that Baltimore and other cities could build on: “We could turn brownfields into health fields by cleaning up contaminated sites and placing health-care facilities there.”—Steve Dubb












