
Community health centers are vitally important within a healthcare landscape where a growing number of Americans can’t access care. These centers offer their services to patients, “regardless of their ability to pay.”
According to the Commonwealth Fund 2024 National Survey of Federally Qualified Health Centers, “[a]cross the United States, federally qualified health centers (FQHCs) provide accessible, comprehensive, and coordinated primary care to more than 30 million patients.” The Commonwealth Fund defines FQHCs as “community-based outpatient clinics that provide primary medical, dental, behavioral, and other health care services.”
Despite the need for community health centers, the Commonwealth Fund’s survey revealed that worker shortages threaten their ability to provide care.
FQHCs use a community-centered model that includes community members on boards, provides high-quality care for chronic conditions like hypertension and Type 2 diabetes, combats the inaccessibility of mental health services by offering behavioral health support, and offers patients transportation. Additionally, through serving rural areas and other traditionally underserved populations, FQHCs play an important role in preventing medical deserts.
When the survey was conducted, in the fall of 2023 to spring of 2024, the Commonwealth Fund identified 1,369 FQHCs operating at 15,000 service sites. The survey, which included 737 community health center leaders, including “executive directors, clinical directors, or project directors,” focused on “the core functions of primary care—accessibility, comprehensiveness, and coordination,” staffing needs, telehealth utilization, and other aspects of care provision. Since this survey was previously conducted in 2018, it also provides comparative data on how community health centers have changed over the last six years.
Worker Shortages
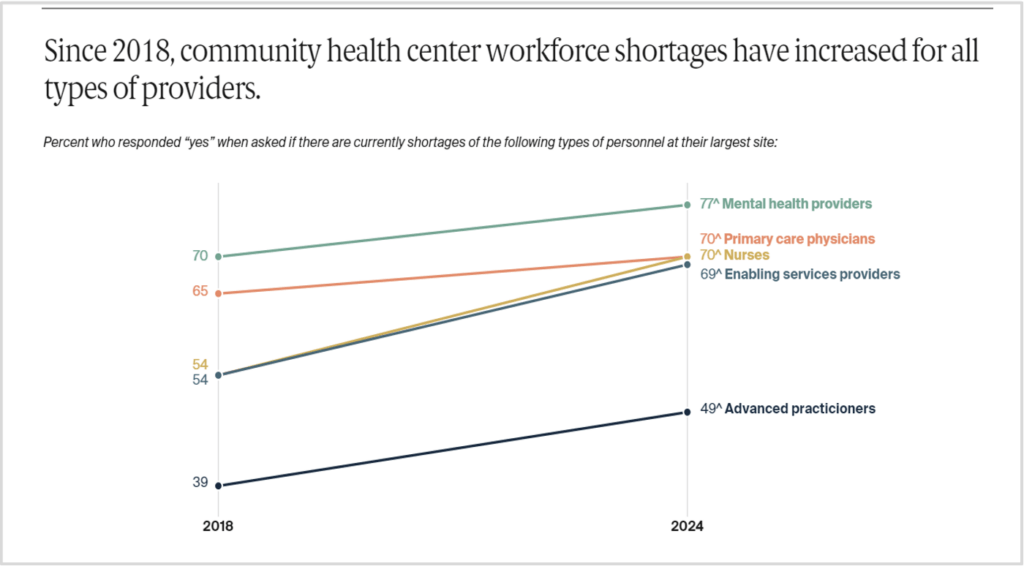
Despite the need for community health centers, the Commonwealth Fund’s survey revealed that worker shortages threaten their ability to provide care. From 2018 to 2024 a significant majority of community health workers reported staffing shortages in key areas.
In 2024, approximately 77 percent of community health center leaders reported a shortage in mental health providers, roughly 70 percent of leaders reported shortages in primary care physicians and nurses, and around 69 percent reported a shortage in enabling service providers.
Almost half (49 percent) of community health center leadership said they were currently experiencing a staffing shortage in advanced practitioners—a classification that includes nurse practitioners and physician assistants.
While the root causes of these staffing shortages were not directly addressed in the survey, according to the Commonwealth Fund, competition with larger health systems that provide higher pay for medical professionals could be one of the main drivers of the staffing shortages at community health centers. Additionally, community health centers may continue to suffer the ramifications of healthcare provider burnout and distress accompanying the height of the COVID-19 pandemic.
Telehealth Use Is on the Rise at Community Health Centers
According to the surveyed community health center leaders, telehealth has become a useful tool for overburdened centers to continue to serve patients.
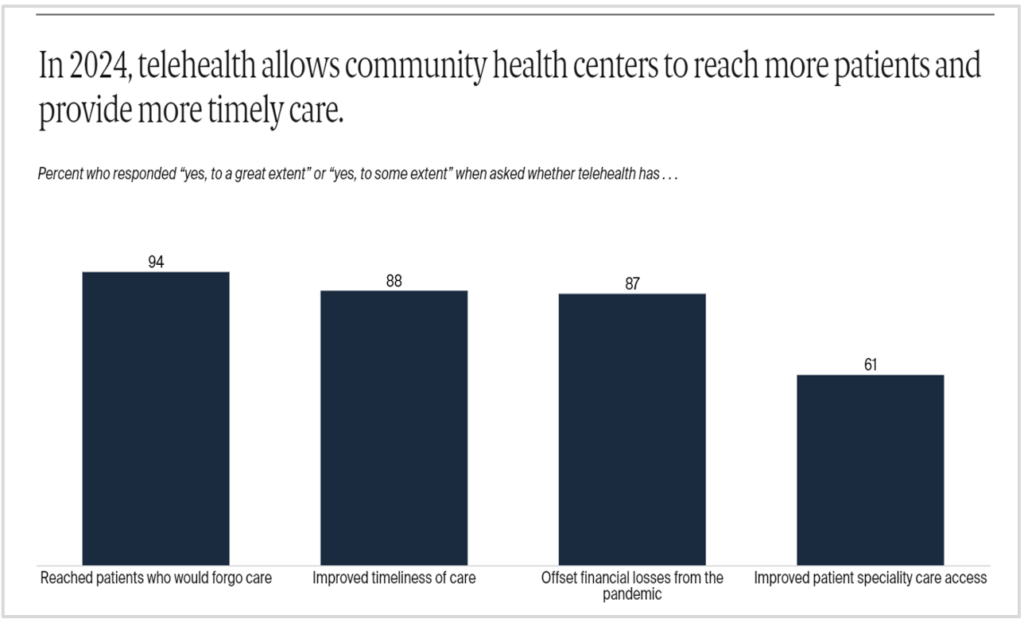
Approximately 94 percent of community health center leaders said that telehealth reached patients who would otherwise forgo care. Around 88 percent of leaders say that telehealth improved the timeliness of care. Around 87 percent of leaders said that telehealth helped their centers offset financial losses from the pandemic. And more than half, or 61 percent, of community health center leaders said that telehealth improved their patients’ access to specialty care.
Telehealth has become an effective tool for overburdened centers.
Even though the Commonwealth Fund’s survey suggests that telehealth effectively extends the reach of community health centers, much of the research on the utility of telehealth (especially for marginalized and otherwise underserved populations), asserts that the tech carries both benefits and drawbacks.
Community Health Centers Are Integral to Health Equity
Community health centers continue to set national standards in providing equitable and comprehensive care. They accomplish this by understanding their patients’ social and economic needs, providing care in a variety of languages and modalities, and coordinating with community-based organizations.
Sign up for our free newsletters
Subscribe to NPQ's newsletters to have our top stories delivered directly to your inbox.
By signing up, you agree to our privacy policy and terms of use, and to receive messages from NPQ and our partners.
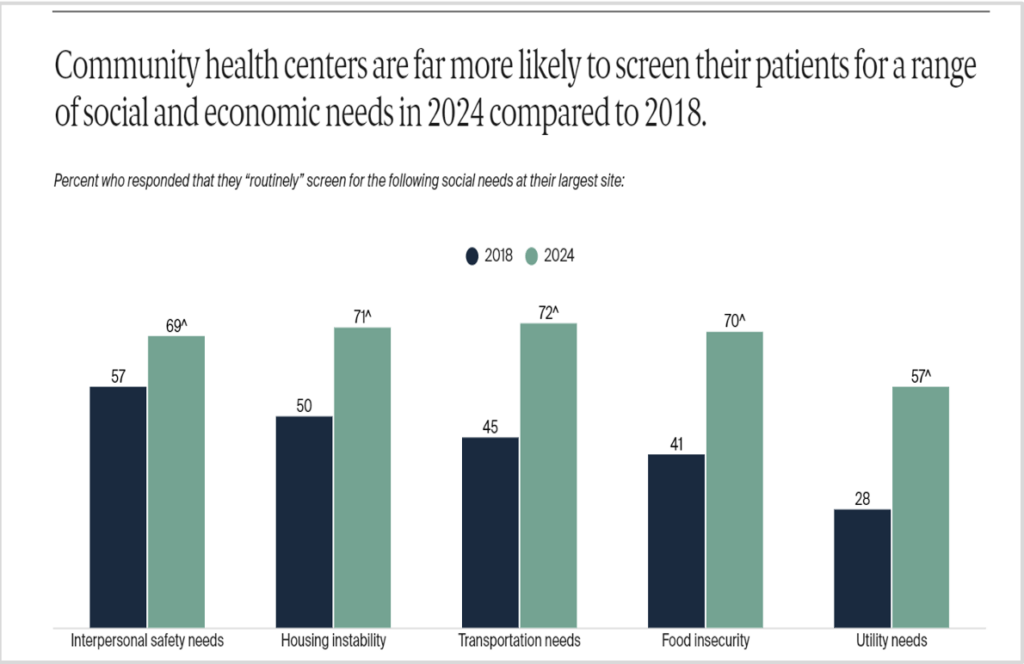
In 2024, community health center leaders reported significant increases in social and economic screening activity compared to 2018. Approximately 69 percent of leaders said that their community health center screens for patients’ interpersonal safety needs, up from around 57 percent in 2018. And about 71 percent of community health center leaders said they screen for housing instability, which has risen from 50 percent in 2018.
In 2024, 72 percent of community health center leaders said they screened for transportation needs, compared to 45 percent in 2018. Similarly, more community health centers reported screening for food security in 2024 (70 percent) than in 2018 (41 percent). Currently, about 57 percent of community health centers’ leaders report screening for utility needs versus only 28 percent in 2018.
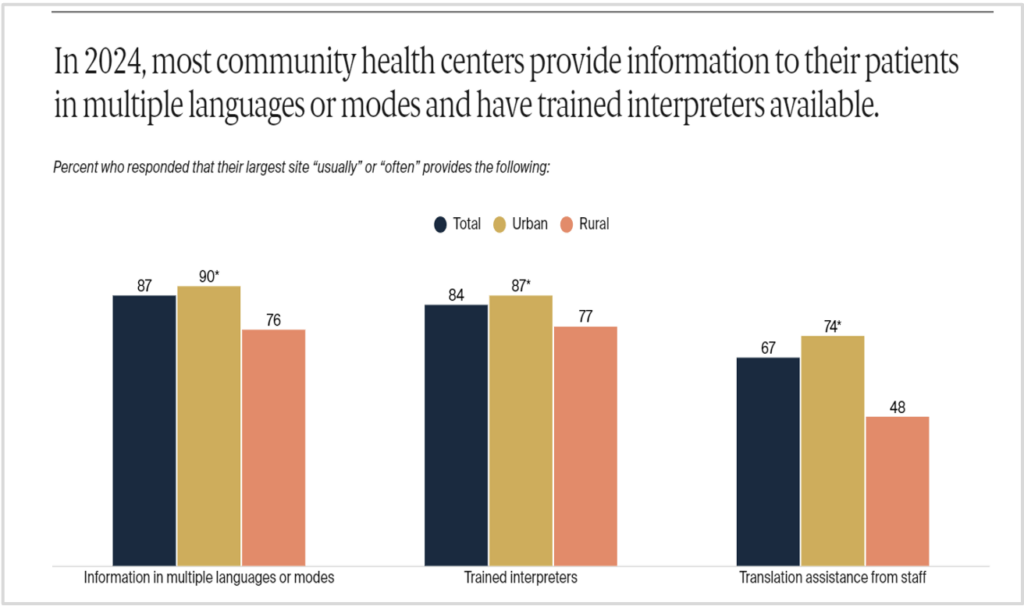
In 2024, most community health center leaders (90 percent) reported offering their services in a variety of languages and modes. The percentage of community health centers that reported having trained interpreters on site was also high at 87 percent, and translation assistance from staff came in at around 74 percent.
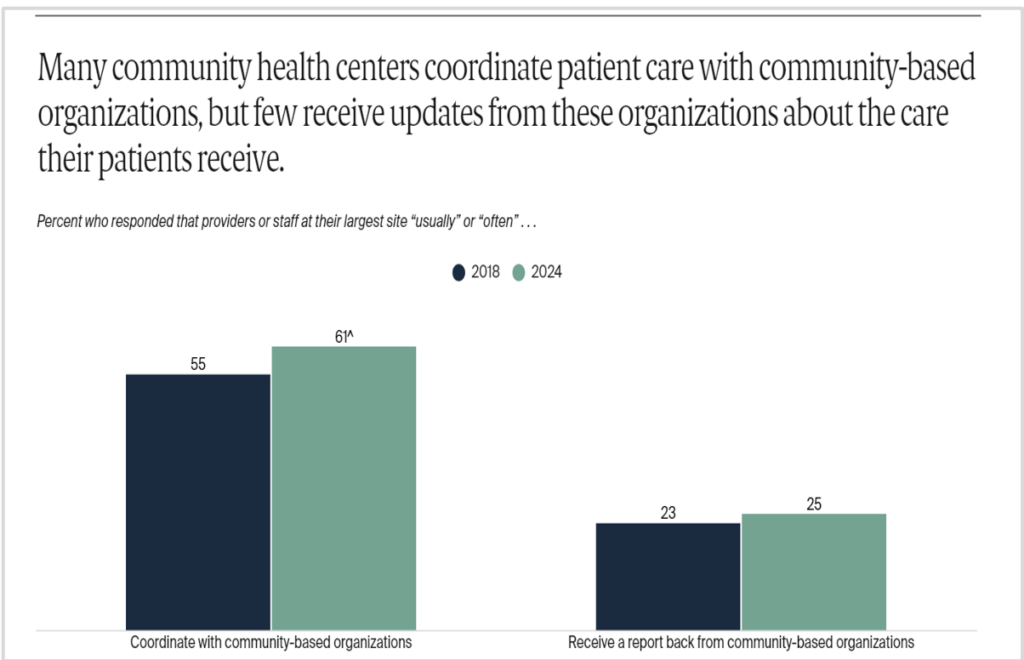
Between 2018 and 2024, community health centers also significantly increased coordination of care with community-based organizations. In 2018, a little more than half, or 55 percent, of community health center leaders said that they coordinated with community-based organizations. This number rose modestly in 2024, now at 61 percent. According to the data, approximately 25 percent of community health centers said they received reports from these community-based organizations, compared with just 23 percent of FQHCs who said they received reports in 2018.
Community health centers continue to set national standards in providing equitable and comprehensive care.
The survey data also suggest that inadequate staffing for community-based organizations and inadequate social service resources in the community make it difficult to meet patients’ “unmet needs.”
More Support Is Needed to Continue Community-Centered Care
The Commonwealth Fund argues that “[d]espite their progress, community health centers face challenges that threaten their ability to continue offering high-quality care.”
For the 30 million patients served by community health centers, these facilities are a lifeline. But through disinvestment in their communities, these centers—as well as the community-based organizations that coordinate with them to offer comprehensive care and address the social determinants of health—are on shaky financial ground. Unlike many other health systems whose revenue is generated through Medicare and private insurance reimbursements, community health centers rely on much lower Medicaid reimbursements.
According to data from the Harvey L. Neiman Health Policy Institute, though reimbursements differ throughout the country, Medicaid reimbursement rates are on average only 78 percent of Medicare reimbursement rates. Increasing Medicaid reimbursements is critical to ensure that low-income Americans have access to healthcare and that community-centered services are available for the people who need them the most.
One of the Commonwealth Fund’s key recommendations for addressing the critical staffing shortages and other needs of community health centers is to reauthorize and extend the Community Health Center Fund. The fund, which is periodically reauthorized by Congress, is set to expire at the end of 2024. According to research from the Congressional Budget Office, reallocating and bolstering the Community Health Center Fund would save the federal government money in the long run by lowering high-cost healthcare utilization tied to devasting health events like heart attacks, which can be avoided with proper preventative care.
The Commonwealth Fund also calls on Congress to “expand recruitment, retention, and training programs that encourage providers to practice in medically underserved or rural areas, such as the National Health Service Corps and the Teaching Health Center Graduate Medical Education Program.” As NPQ has discussed, if programs are not specifically designed to increase the number of primary care physicians and specialties experiencing shortages, and if these programs don’t require healthcare providers to practice in underserved areas, investments in expanding the healthcare workforce won’t translate to change.
As healthcare costs continue to rise, change is desperately needed. With more financial support, community health centers can continue to do what they do best: offer healthcare and social support to the people otherwise shut out of America’s healthcare system.












