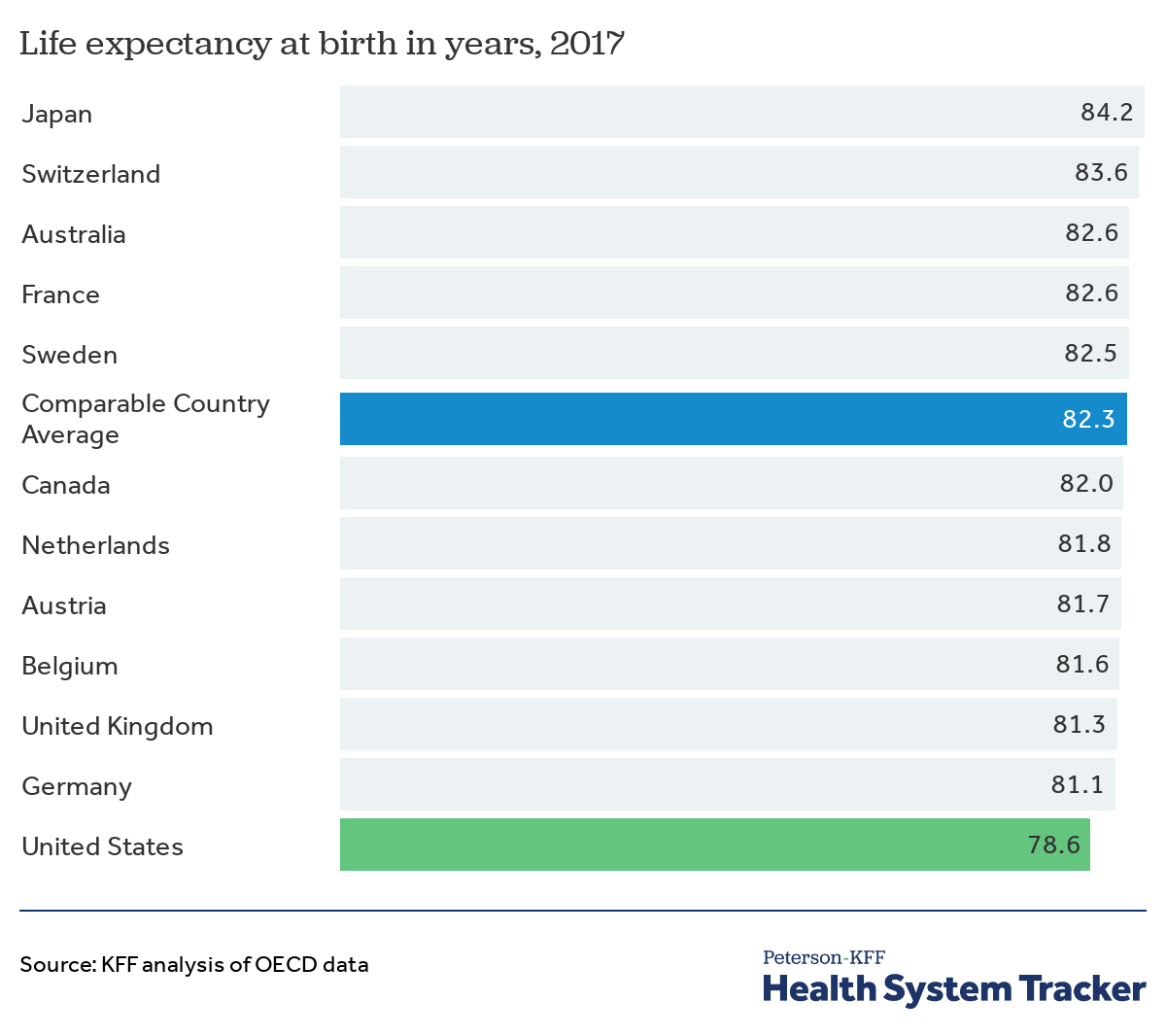
Building on a set of articles in the winter 2020 issue of Nonprofit Quarterly, this webinar in our Remaking the Economy series looks at healthcare, the largest sector of the US economy. Famously, the US pays far more than any other nation on healthcare—17.7 percent of the economy in 2019—yet has inferior health outcomes. The Peterson Center on Healthcare and Kaiser Family Foundation report that “Back in 1980, life expectancy at birth in the US was similar to that of comparable countries. However, since then, the US has gained just 4.9 years of life expectancy, while comparable countries have gained 7.8 years on average.” The average American now lives 2.5 years less long than the average German and 5.6 years less long than the average Japanese person.
Economic inequality and racism are two drivers of poor US health outcomes. This year, the American Medical Association formally recognized racism as a public health threat. The impact of racism in health care can be seen in age-adjusted COVID-19 mortality rates for Black, Latinx, and Native Americans, which are twice that of whites. How can healthcare be retooled to address these disparities and promote better health?
In this webinar, we feature three panelists who address these issues:
Ben Palmquist is program director of health care and economic democracy for Partners for Dignity and Rights, a New York City-based nonprofit that advocates for a new social contract where everyone’s human needs are met.
Al Richmond is based in Raleigh, North Carolina, and is executive director of Community-Campus Partnerships for Health, a member-based nonprofit that promotes health equity and social justice through partnerships between communities and academic institutions.
Yolandra Toya, MD, MPH is a physician and community pediatrician, and a citizen of the Jicarilla Apache nation. In her practice, Dr. Toya is currently providing medical care to residents of both Native and non-Native communities in New Mexico.
Among the questions covered in a wide-ranging conversation are the following:
Sign up for our free newsletters
Subscribe to NPQ's newsletters to have our top stories delivered directly to your inbox.
By signing up, you agree to our privacy policy and terms of use, and to receive messages from NPQ and our partners.
- What are some of the leading structural causes of healthcare injustice in the United States? What can be done to address them?
- What does good community-based health research look like? How does poorly conducted health research in the past continue to sow mistrust in the present?
- How do you approach Native communities if you want to engage in health promotion work?
- What are social determinants of health and how do you address them?
- What are existing protective factors within communities of color that can be reinforced to achieve better health outcomes?
- How do communities gain greater control over their own health care?
- Is COVID-19 teaching us new things about healthcare in the US, or is it mostly confirming what was already known?
- How do we prepare for addressing the aftereffects of “long COVID”?
- What are policy steps that the new administration can take in Washington?
Resources
Articles by or about the panelists
Kathleen McCleery, “Needed: Native Doctors—Yolandra Gomez Toya ’88 works to close the gap,” Princeton Alumni Weekly, March 7, 2018.
Lloyd Michener, Sergio Aguilar-Gaxiola, Philip M. Alberti, Manuel J. Castaneda, Brian C. Castrucci, Lisa Macon Harrison, Lauren S. Hughes, Al Richmond, and Nina Wallerstein, “Engaging with Communities—Lessons (Re)Learned from COVID-19,” Preventing Chronic Disease, July 2020.
Ben Palmquist, “The Struggle for Healthcare Justice: It’s Movement Time,” NPQ, January 14, 2021.
Additional resources
Karen Kahn, “Crisis within a Crisis: Health Workers on the Front Line of COVID-19,” NPQ, January 15, 2021.
Ruth McCambridge, “Profit as Primary Driver: The Daily Disaster of U.S. Healthcare,” NPQ, January 19, 2021.
The Editors, “Recognizing Racism as a Public Health Threat: A Conversation with Dr. Willarda V. Edwards,” NPQ, January 22, 2021.
Steve Dubb, “Communities Must Engage to Improve Health Outcomes,” NPQ, November 15, 2017.













