August 30, 2018; Healthcare Dive
Moody’s says that even as some nonprofit health systems prosper, others are falling short. According to Les Masterson in Healthcare Dive, the Moody’s report indicates that “28.4 percent of nonprofit hospital experienced operating losses, an increase from 16.5 percent in 2016. Also, 59 percent of providers reported lower absolute operating cash flow, which was more than double the 24 percent noted in 2015. The 2017 figure was the highest percentage in five years.”
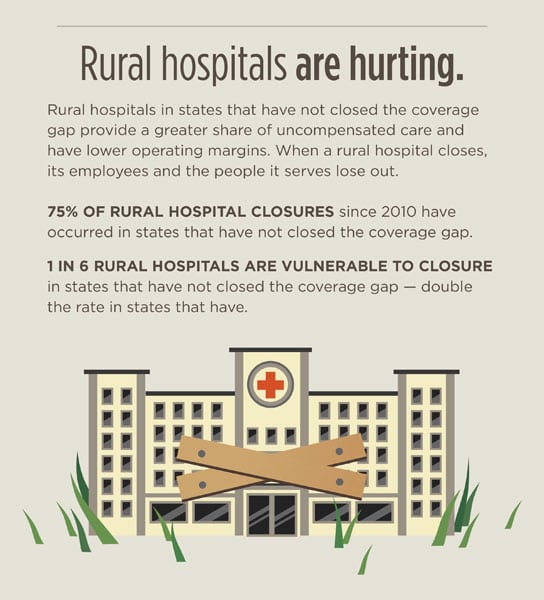
Of these troubled nonprofit health systems, rural hospitals face the greatest challenges. Since 2010, the University of North Carolina’s Cecil G. Sheps Center for Health Service Research has recorded 87 rural hospital closures in more than 20 states. According to one study, an additional 673 hospitals are vulnerable to closing, located across 42 states, with an estimated 99,000 jobs at stake. Nearly 12 million patients could lose direct access to care.
Why this perilous scenario for rural hospitals? First, rural hospitals serve populations that tend to have higher rates of chronic illness than those served by urban hospitals. Their patients are older and poorer, and 60 percent of rural hospitals’ revenues are from Medicare and Medicaid, compared with 45 percent for urban facilities. Second, even small changes in federal programs can have a disproportionate effect on the financial viability of these hospitals. The Affordable Care Act, for example, cut funding for uncompensated care and forced rural residents facing the prospect of having only one insurer on the exchange into high-deductible health plans. Third, rural hospitals are often small, with aging facilities; they commonly have lower occupancy rates and may struggle to attract physicians. Interestingly, a recent study found that rural hospitals saw an improved chance of turning a profit if they were in one of the 34 states that chose to expand Medicaid.
Sign up for our free newsletters
Subscribe to NPQ's newsletters to have our top stories delivered directly to your inbox.
By signing up, you agree to our privacy policy and terms of use, and to receive messages from NPQ and our partners.
Patrick County sits in mountainous southwest Virginia, bordering North Carolina. With a population of 18,000 (a nearly five percent drop from 2010) and a 22-percent poverty rate (compared to 11 percent for the state), its 60-year-old hospital has struggled to make ends meet. Residents were horrified to abruptly learn a year ago that their only hospital was closing its doors, putting 140 employees out of work and extending the average ambulance trip from 30 minutes to two-to-three hours. The Patrick County rescue squad, like most rural emergency providers, is almost entirely made up of volunteers who work full-time jobs and can’t afford to take the additional time off to transport emergency patients. The hospital’s closing has also put a dent in the county’s increasing success at attracting retirees to settle in the community.
In early 2016, the hospital’s Mississippi-based owner, Pioneer Health Services, filed for Chapter 11 bankruptcy. Virginia Community Capital (VCC), the hospital’s largest creditor, which made a $6.5 million loan to the hospital in 2013 for renovations, is now its interim owner and is asking at least $5 million for the property. Created under then-Democratic Governor Mark Warner, VCC is known as an innovative community development financial institution that has leveraged millions from national and state social investors for affordable housing, small businesses, and healthcare in underserved parts of the state. Patrick County Board of Supervisors Chair Lock Boyce, however, believes the hospital is worth no more than $2 million and proposes that VCC lease the facility to the county, which would then find someone to operate it as a hospital. But time is running out, with the hospital’s license as a 25-bed acute facility set to expire at the end of 2018, and the state’s May 31, 2018, decision to finally expand Medicaid may have come too late to help this rural hospital.
Rural hospitals, even those that are privately owned, seem like public assets to their residents. Patrick County citizens raised $300,000 in the late 1950s—some giving small but personally significant donations—to fund half the costs of the hospital’s construction. But rural hospitals are hybrids—part social welfare organization, part business—and it is this contradiction that remains unresolved, leaving this country’s rural people hit hard.—Debby Warren













